2013年9月30日星期一
COPD exacerbation
80 year old female with past history of moderate COPD( 3L oxygen all the time), HTN, hyperlipidemia, osteoporosis, glaucoma and CAD present with shortness of breath since yesterday morning. Patient is getting SOB every day in the morning since last month. She has been taking Proair(albuterol) and Duoneb (albuterol/ipratropium), SOB normally can improve and go back to baseline within 1 hour. yesterday morning, her SOB couldn't improve with same medications, therefore, she came to ER. She had COPD exacerbation in Dec 2012, Mar 2013. She has always cough with clear phlegm. there is no fever, chills, no chest pain, orthopnea, paroxysmal nocturnal dyspnea. She smoke all her life for 60-70 years, but quit smoking 2 weeks ago. at ER, she received solu medrol 125 mg IV once, and Duoneb once.
vital, RR 22, SaO2 95% on 3L, cxr no acute infiltrate, EKG is normal sinus rhythm.
assessment and plan:
1, COPD exacerbation, solu medrol 60mg IV q8h, for 1-2 days, then transtion to po steroid, plus azithromycin 500mg once for 3 days.
2, HTN, continue lisinopril and metoprolol
3, CAD, continue ACEi, beta blocker, aspirin and statin
4, start omeprazol as she will be on steroid.
Management of acute exacerbations of chronic obstructive pulmonary disease
defines an exacerbation of chronic obstructive pulmonary disease (COPD) as an acute increase in symptoms beyond normal day-to-day variation. This generally includes an acute increase in one or more of the following cardinal symptoms:
■Cough increases in frequency and severity
■Sputum production increases in volume and/or changes character
■Dyspnea increases
Constitutional symptoms, an unchanged chest radiograph, a variable decrease in pulmonary function, and tachypnea are typical in acute exacerbations
Rapid overview: Emergency management of severe acute COPD exacerbations
General points
Chronic obstructive pulmonary disease (COPD) exacerbations are most often precipitated by infection (viral or bacterial)
Differential diagnosis includes: Acute decompensated heart failure, pulmonary embolism (PE), pneumonia, pneumothorax
Clinical manifestations
Cardinal symptoms: Increase or change in character of dyspnea, cough, sputum production
Diagnostic testing
Assess oxygen saturation with pulse oximetry
Obtain arterial blood gas in severe exacerbations
Obtain chest radiograph to assess for signs of pneumonia, acute heart failure, pneumothorax
Obtain complete blood count and measures of basic electrolytes and renal function
Obtain electrocardiogram
Pharmacotherapy
Oxygen to target saturation of 90 to 94 percent and PaO2 of 60-70 mmHg; Venturi mask can be useful for titrating FiO2; high FiO2 usually not needed and can contribute to hypercapnia (high FiO2 requirement should prompt consideration of alternative diagnosis (eg, PE))
Inhaled beta agonist (eg, albuterol 2.5 mg diluted to 3 mL via nebulizer)
Inhaled anticholinergic agent (eg, ipratropium 500 micrograms via nebulizer)
Systemic corticosteroid (eg, methylprednisolone 60 mg IV)
Antibiotic therapy: Levofloxacin (750 mg IV) or alternative based on likely pathogens (including risk of pseudomonas infection) and local patterns of antibiotic resistance
Noninvasive Positive Pressure Ventilation (NPPV)
Indicated for moderate to severe exacerbations
Use only if tracheal intubation not immediately necessary and no other contraindications
Contraindications to NPPV include: Severely impaired consciousness, inability to clear secretions or protect airway, high aspiration risk
Initial settings for bilevel NPPV: 8 cm H2O inspiratory pressure (may increase up to 15 cm H2O if needed to aid ventilation); 3 cm H2O expiratory pressure
Monitoring and initial interventions
Perform continual monitoring of oxygen saturation, cardiac rhythm, and vital signs
Place two peripheral IV catheters
Tracheal intubation
For patients with severe respiratory distress in whom NPPV is contraindicated or who fail to improve with NPPV and aggressive pharmacotherapy
Disposition
Criteria for hospitalization include:
Patients with high-risk comorbidities (pneumonia, cardiac arrhythmia, heart failure, diabetes mellitus, renal failure, liver failure)
Inadequate improvement of symptoms with initial therapies
Marked increase in dyspnea
Inability to eat or sleep due to symptoms
Worsening hypoxemia or hypercapnea
PRECIPITANTS — It is estimated that 70 to 80 percent of COPD exacerbations are due to respiratory infections, including:
Haemophilus influenzae 13 to 50
Moraxella catarrhalis 9 to 21
Streptococcus pneumoniae 7 to 26
Pseudomonas aeruginosa 1 to 13
The remaining 20 to 30 percent are due to environmental pollution or have an unknown etiology.
The single best predictor of exacerbations was a history of exacerbations, regardless of COPD severity.
The GOLD guidelines suggest using a combination of an individual’s FEV1 and history of exacerbations to assess the exacerbation risk [1]. The number of exacerbations in the previous 12 months is stratified: a history of zero or one exacerbation suggests a low future risk of exacerbations, while two or more suggest a high future risk.
Severity of airflow limitation in COPD (based on postbronchodilator FEV1)
In patients with FEV1/FVC <0.7:
GOLD 1 Mild FEV1 ≥80 percent predicted
GOLD 2 Moderate 50 percent ≤FEV1 <80 percent predicted
GOLD 3 Severe 30 percent ≤FEV1 <50 percent predicted
GOLD 4 Very severe FEV1 <30 percent predicted
■Low risk: Typically GOLD 1 or 2 (mild to moderate airflow limitation) and/or 0 to 1 exacerbation per year
■High risk: Typically GOLD 3 or 4 (severe or very severe airflow limitation) and/or ≥2 exacerbations per year
DIFFERENTIAL DIAGNOSIS — Patients with COPD who present to the hospital with acute worsening of dyspnea should be evaluated for potential alternative diagnoses, such as heart failure, pulmonary thromboembolism, and pneumonia.
TREATMENT:
OXYGEN THERAPY — Supplemental oxygen is a critical component of acute therapy. It should target an arterial oxygen tension (PaO2) of 60 to 70 mmHg, with an oxyhemoglobin saturation of 90 to 94 percent.
PHARMACOLOGIC TREATMENT — The major components of managing an acute exacerbation of COPD include inhaled short-acting bronchodilators (beta adrenergic agonists and anticholinergic agents), glucocorticoids, and antibiotics.
Beta adrenergic agonists — Inhaled short-acting beta adrenergic agonists (eg, albuterol) are the mainstay of therapy for an acute exacerbation of COPD.These medications may be administered via a nebulizer or a metered dose inhaler (MDI) with a spacer device.
Despite evidence that MDI devices may have equal efficacy during acute exacerbations of COPD, many clinicians prefer nebulized therapy on the presumption of more reliable delivery of drug to the airway [1]. We favor nebulized therapy because many patients with COPD have difficulty using proper MDI technique in the setting of an acute exacerbation.
Patients with severe COPD are at risk for hypercapnia with administration of supplemental oxygen, so concern has been raised about the risk of hypercapnia during bronchodilator treatments using oxygen-driven nebulizers.We concur with the British Thoracic Society guidelines that suggest using air-, rather than oxygen-driven bronchodilator nebulization, or limiting oxygen-driven treatments to 6 minutes.
Anticholinergic agents — Inhaled short-acting anticholinergic agents (eg, ipratropium bromide) are used with inhaled short-acting beta adrenergic agonists to treat exacerbations of COPD.
Glucocorticoids
Route — Oral glucocorticoids are rapidly absorbed (peak serum levels achieved at one hour after ingestion) with virtually complete bioavailability and appear equally efficacious as intravenous glucocorticoids for treating most exacerbations of COPD. As an example, a randomized trial assigned 210 patients hospitalized with a COPD exacerbation to receive oral or intravenous prednisolone (60 mg daily) for five days and found no difference between the two groups in the rate of treatment failure, length of hospital stay, improvement in spirometry, or improvement in quality of life. However, intravenous glucocorticoids are typically administered to patients who present with a severe exacerbation, who respond poorly to oral glucocorticoids, who are unable to take oral medication, or who may have impaired absorption due to decreased splanchnic perfusion (eg, patients in shock).
Antibiotics — Antibiotics are indicated for many patients having a COPD exacerbation.
CHEST PHYSIOTHERAPY — Mechanical techniques to augment sputum clearance, such as directed coughing, chest physiotherapy with percussion and vibration, intermittent positive pressure breathing, and postural drainage, have not been shown to be beneficial in COPD and may provoke bronchoconstriction. Their use in acute exacerbations of COPD is not supported by clinical trials.
MECHANICAL VENTILATION
Noninvasive ventilation — Noninvasive positive pressure ventilation (NPPV) refers to mechanical ventilation delivered through a noninvasive interface, such as a face mask, nasal mask, or nasal prongs. It improves numerous clinical outcomes and is the preferred method of ventilatory support in many patients with an acute exacerbation of COPD.
Invasive ventilation — Invasive mechanical ventilation should be administered when patients fail NPPV, do not tolerate NPPV, or have contraindications to NPPV.
PROGNOSIS — Acute exacerbations of COPD are associated with increased mortality after hospital discharge.
■It is estimated that 14 percent of patients admitted for an exacerbation of COPD will die within three months of admission [47,48].
■Among 1016 patients with an acute exacerbation of COPD and a PaCO2 of 50 mmHg or more, the 6 and 12 month mortality rates were 33 and 43 percent, respectively [49].
■In a study of 260 patients admitted with a COPD exacerbation, the one year mortality was 28 percent [50]. Independent risk factors for mortality were age, male gender, prior hospitalization for COPD, PaCO2 ≥45 mmHg (6 kPa), and urea >8 mmol/L.
■Patients hospitalized for a COPD exacerbation who have a Pseudomonas aeruginosa in their sputum have an increased risk of mortality at three years than those without (59 versus 35 percent, HR 2.33, 95% CI 1.29-3.86), independent of age, comorbidity, or COPD severity
SUMMARY AND RECOMMENDATIONS
■A table to assist with emergency management of severe acute exacerbations of COPD is provided (table 1).
■An acute exacerbation of COPD is characterized by an acute increase in symptoms beyond normal day-to-day variation. (See 'Introduction' above.).
■We recommend that all patients having a COPD exacerbation receive both an inhaled short-acting beta adrenergic agonist and an inhaled short-acting anticholinergic agent, rather than either medication alone (Grade 1B). (See 'Beta adrenergic agonists' above and 'Anticholinergic agents' above.)
■We recommend that all patients having a COPD exacerbation receive systemic glucocorticoids (Grade 1A). A reasonable dose for patients not requiring intensive care unit admission is prednisone 30 to 60 mg orally once daily, or the equivalent, for 10 to 14 days, although preliminary data suggest that a 5 day course may be an acceptable alternative. (See 'Glucocorticoids' above.)
■Antibiotics are indicated for many patients having a COPD exacerbation. (See "Management of infection in acute exacerbations of chronic obstructive pulmonary disease", section on 'Summary and recommendations'.)
■Mucoactive agents, mechanical techniques to augment sputum clearance, and methylxanthines have not been shown to confer benefit for patients with a COPD exacerbation. (See 'Mucoactive agents' above and 'Chest physiotherapy' above and 'Methylxanthines' above.)
■We suggest that all patients who are hypoxemic be given supplemental oxygen targeting a PaO2 of 60 to 70 mmHg, with an oxyhemoglobin saturation of 90 to 94 percent (Grade 2C). (See 'Oxygen therapy' above.)
■Noninvasive positive pressure ventilation (NPPV) improves numerous clinical outcomes and is the preferred method of ventilatory support in many patients with an acute exacerbation of COPD. Invasive mechanical ventilation is required in patients with respiratory failure who fail NPPV, do not tolerate NPPV, or have contraindications to NPPV. Both NPPV and invasive mechanical ventilation for patients with an acute exacerbation of COPD are discussed separately.
Initial management of animal and human bites
INTRODUCTION — Animal and human bites are a common problem. Proper care requires wound inspection for injury to deeper structures; meticulous wound care at the initial encounter; and decisions regarding primary closure, the provision of prophylactic antibiotics for wounds at high risk for infection, and prophylaxis for tetanus and rabies as indicated.
EPIDEMIOLOGY — Animal bites are common. In the United States, there is an annual incidence of two to five million occurrences which account for about 1 percent of all visits to emergency departments. Approximately 10 percent of bite wounds presenting for medical attention require suturing and follow-up care, and 1 to 2 percent result in hospitalization.
MICROBIOLOGY — The predominant pathogens in animal bite wounds are the oral flora of the biting animal and human skin flora. Infection usually results from a mixture of organisms. Common pathogens (in order of prevalence) include Pasteurella species, staphylococci, streptococci, and anaerobic bacteria. Capnocytophaga canimorsus, a fastidious gram-negative rod, can cause bacteremia and fatal sepsis after animal bites, especially in asplenic patients, chronic alcohol abusers, or those with underlying hepatic disease. Cat bites can also transmit Bartonella henselae, the organism responsible for cat scratch disease.
Cat bites — Two-thirds of cat bites involve the upper extremities; scratches typically occur on the upper extremities or face. Deep puncture wounds are of particular concern because cats have long, slender, sharp teeth. When the hand is the target of such a puncture wound, bacteria can be inoculated below the periosteum or into a joint and result in osteomyelitis or septic arthritis
INITIAL MANAGEMENT:
Stabilization — Direct pressure should be applied to actively bleeding wounds and a neurovascular assessment should be performed in areas distal to the wound. Deep wounds to vital structures should be treated as major penetrating trauma.
Wound preparation — Appropriate local anesthesia facilitates adequate wound cleansing. To reduce the counts of bacteria present in the wound, the surface should be cleaned with 1 percent povidone iodine or 1 percent benzalkonium chloride, and the depths irrigated with copious amounts of saline using pressure irrigation. Debridement of devitalized tissue is important to remove any nidus for infection.
Primary closure — A clinician with prior training and experience in laceration repair may perform primary wound closure of simple lacerations due to dog bites. In contrast, most cat or human bites are left open to heal by secondary intention. In addition to these indications for primary wound closure of open lacerations, we suggest that the laceration meets ALL of the following criteria:
■Clinically uninfected
■Less than 12 hours old (24 hours on the face)
■NOT located on the hand or foot
In particular, wounds to the face are usually closed promptly because good cosmesis is especially important, and infection of these wounds is uncommon
Wounds at high risk for the development of infection should NOT be closed primarily in most cases [3,5,8,29,30]. These include:
■Crush injuries
■Puncture wounds
■Bites involving the hands and feet
■Wounds more than 12 hours old (24 hours old on face)
■Cat or human bites, except those to the face
■Bite wounds in compromised hosts (eg, immunocompromised, absent spleen or splenic dysfunction, venous stasis, diabetes mellitus [adults])
Surgical consultation — Surgical consultation is usually necessary for the following wounds [30]:
■Deep wounds that penetrate bone, tendons, joints, or other major structures
■Complex facial lacerations
■Wounds associated with neurovascular compromise
■Wounds with complex infections (eg, abscess formation, osteomyelitis, or joint infection)
Antibiotic prophylaxis — Prophylactic antibiotics reduce the rate of infection due to some animal bites, especially cat bites. Although routine antibiotic prophylaxis is not recommended, prophylaxis is warranted in certain high-risk wounds .
■Deep puncture wounds (especially due to cat bites)
■Moderate to severe wounds with associated crush injury
■Wounds in areas of underlying venous and/or lymphatic compromise
■Wounds on the hand(s), genitalia, face, or in close proximity to a bone or joint (particularly the hand and prosthetic joints)
■Wounds requiring closure
■Bite wounds in compromised hosts (eg, immunocompromised, absent spleen or splenic dysfunction, and adults with diabetes mellitus)
Tetanus and rabies prophylaxis —
Viral prophylaxis after human bites — Any unvaccinated patient or individual negative for anti-HBs antibodies who is bitten by an individual positive for HBsAg should receive both hepatitis B immune globulin (HBIG) and hepatitis B vaccine
Infected bites — To successfully manage an infected wound, the clinician must recognize early signs of infection and be aware of the likely pathogens. (See 'Infected wound' above.)
If a bite wound appears to be infected, the following actions should be taken:
■Remove suture material, if previously repaired.
■Obtain Gram stain and aerobic and anaerobic cultures from the depth of an infected puncture or laceration prior to the initiation of antibiotics. The laboratory requisition should note that an animal or human bite wound is the culture source.
■Draw aerobic and anaerobic blood cultures prior to antibiotic therapy in patients with signs of systemic infection.
■Consult a surgeon for possible operative exploration, debridement, and drainage if abscess formation or suspected infection of bone, joint, or other major underlying structure (eg, clenched fist infections and other hand infections) is present. Debrided material should be sent for aerobic and anaerobic culture.
■Hospitalize patients with systemic symptoms or progression or development of infection despite receiving oral antibiotics.
Empiric antibiotic therapy — Once a bite becomes infected, it is crucial to perform aggressive debridement and abscess drainage, as indicated, and to administer intravenous broad-spectrum antibiotics to cover probable infecting bacteria in patients with dog or cat bites (table 1) or human bites (table 2). A common approach involves initial IV therapy until infection is resolving followed by oral therapy to complete a course of 10 to 14 days.
Empiric intravenous antibiotic therapy for animal bites
Adults Children
Options for empiric gram-negative and anaerobic coverage include:
Monotherapy with a beta-lactam/beta-lactamase inhibitor, such as one of the following:
Ampicillin-sulbactam (unasyn) 3 g every six hours 50 mg/kg per dose (based on ampicillin component) every six hours*
Piperacillin-tazobactam (zosyn)4.5 g every eight hours 125 mg/kg per dose (based on piperacillin component) every eight hours*
Ticarcillin-clavulanate (timentin)3.1 g every four hours 50 mg/kg per dose (based on ticarcillin component) every four hours*
A third generation cephalosporin such as ceftriaxone 1 g IV every 24 hours PLUS Metronidazole 500 mg IV every eight hours
A third generation cephalosporin such as ceftriaxone 100 mg/kg per dose every 24 hours* PLUS Metronidazole 10 mg/kg per dose every eight hours*
COMPLICATIONS — The most serious complications of animal bites include trauma to deep structures, and infections, either transmitted or arising in the wound. In addition children who have suffered dog bites requiring at least minor surgical intervention may develop symptoms of post-traumatic stress disorder (PTSD) [40].
■Systemic infections – Any infected bite wound can progress to infection of underlying structures (eg, bone, joint, tendon) and to bloodstream infection.
Human bites can transmit numerous other infections, including hepatitis viruses B (HBV) and C (HCV), primary syphilis (rare), and herpes simplex virus [33,41].
The risk for transmitting HIV through saliva is extremely low but is of concern if there is blood in the saliva. Counseling regarding post-exposure HIV prophylaxis is appropriate in this setting [34]. (See "Management of healthcare personnel exposed to HIV".)
Any patient negative for anti-HBs antibodies who is bitten by an individual positive for HBsAg should receive both hepatitis B immune globulin (HBIG) and hepatitis B vaccine (table 7). Individuals who work in facilities where the risk for human bites is high, such as institutions for the cognitively impaired, should be given the hepatitis B vaccine series upon employment. (See "Hepatitis B virus vaccination", section on 'Indications'.)
■Post-traumatic stress disorder – Children who have suffered dog bites requiring at least minor wound repair, particularly if the wounds are deep or multiple, may develop symptoms of post-traumatic stress disorder (PTSD) [40]. In one prospective study, the parents of 22 children who presented to an emergency department for minor surgical treatment of dog bites agreed to complete a questionnaire and undergo a telephone and/or personal interview about the circumstances of the injury and the child's behavior before and after it occurred. The interviews took place between two and nine months after the incident. Among the 22 children, 12 had symptoms of PTSD for at least one month (five children met all of the DSM-IV criteria and seven met only some) (table 8).
SUMMARY AND RECOMMENDATIONS
■Most animal bites are caused by dogs, cats, and humans. The predominant organisms in animal bite wounds are the oral flora of the biting animal as well as human skin flora (such as Staphylococci and Streptococci). (See 'Epidemiology' above and 'Microbiology' above and "Soft tissue infections due to dog and cat bites" and "Soft tissue infections due to human bites".)
■The typical location and nature of the injury differs depending upon the animal inflicting the bite. (See 'Clinical manifestations' above.)
Wound assessment
■After appropriate local anesthesia, the wound should be carefully explored to identify injury to underlying structures and the presence of a foreign body. Appropriate imaging should be obtained for deep bite wounds near bone and/or joints and when a foreign body is suspected (eg, plain radiograph or ultrasound). (See 'Plain radiographs and ultrasound' above and "Infiltration of local anesthetics" and "Topical anesthetics in children".)
■Head computed tomography is warranted in patients with a deep dog bite to the scalp, including puncture wounds, especially in children less than two years of age. (See 'Head computed tomography' above.)
■If a bite wound appears to be infected, Gram stain and aerobic and anaerobic cultures should be obtained prior to the initiation of antibiotics. Wound cultures are NOT indicated in clinically uninfected bite wounds as results do not correlate with the likelihood of infection or the pathogen that is present in patients with subsequent infection. (See 'Infected wound' above and 'Wound culture' above.)
Wound management
■Wound irrigation and debridement of devitalized tissue are essential components in the initial management of bite wounds. The wound should be carefully explored to identify injury to underlying structures and the presence of a foreign body. (See 'Wound preparation' above and "Minor wound preparation and irrigation".)
■We suggest primary closure of open lacerations in healthy patients that meet all of the following criteria (Grade 2B):
•Cosmetically important (eg, facial lacerations)
•Wounds that are clinically uninfected
•Wounds less than 12 hours old (24 hours on the face)
•Wounds NOT located on the hand or foot
■Sealing the wound with cyanoacrylate tissue adhesive ("glue") should be avoided. (See 'Primary closure' above and 'Wound preparation' above.)
■We suggest NOT closing wounds at high risk for the development of infection including the following types of wounds (Grade 2C):
•Crush injuries
•Puncture wounds
•Bites involving the hands or feet
•Wounds more than 12 hours old (24 hours old on face)
•Cat or human bites (except those to the face)
•Bite wounds in compromised hosts (eg, immunocompromised, absent spleen or splenic dysfunction, venous stasis, diabetes mellitus [adults]) (see 'Primary closure' above)
■Tetanus and rabies prophylaxis should be provided as indicated. (See 'Tetanus and rabies prophylaxis' above.)
■Surgical consultation may be indicated in selected circumstances. (See 'Surgical consultation' above.)
■Patients who are discharged after initial care should follow-up with their primary care provider or other appropriate clinician within 48 to 72 hours to assess wound status. (See 'Follow-up care' above.)
Antibiotic therapy
■Prophylaxis with oral antibiotics should be given for patient circumstances as outlined above (table 3 and table 4). (See 'Antibiotic prophylaxis' above and "Soft tissue infections due to dog and cat bites", section on 'Prophylaxis' and "Soft tissue infections due to human bites", section on 'Antibiotics'.)
■Patients with deep or severe wound infections are treated with intravenous rather than oral antibiotics (table 1 and table 2). (See 'Infected bites' above and 'Empiric antibiotic therapy' above and "Soft tissue infections due to dog and cat bites", section on 'Prophylaxis' and "Soft tissue infections due to human bites", section on 'Antibiotics'.)
Virus transmission after human bite
■Any patient negative for anti-HBs antibodies who is bitten by an individual positive for HBsAg should receive both hepatitis B immune globulin (HBIG) and hepatitis B vaccine (table 7). (See 'Viral prophylaxis after human bites' above.)
■The risk for transmitting HIV through saliva is extremely low but is of concern if there is blood in the saliva. Counseling regarding post-exposure HIV prophylaxis is appropriate in this setting. (See 'Viral prophylaxis after human bites' above and "Management of healthcare personnel exposed to HIV".)
Cellulitis and erysipelas
CLINICAL MANIFESTATIONS:areas of skin erythema, edema, and warmth. erysipelas involves the upper dermis and superficial lymphatics, whereas cellulitis involves the deeper dermis and subcutaneous fat.erysipelas has more distinctive anatomic features than cellulitis; erysipelas lesions are raised above the level of surrounding skin, and there is a clear line of demarcation. Involvement of the ear (Milian's ear sign) is a distinguishing feature for erysipelas, since this region does not contain deeper dermis tissue. erysipelas tend to have acute onset of symptoms with systemic manifestations including fever and chills; patients with cellulitis tend to have a more indolent course with development of localized symptoms over a few days' time.
DIAGNOSIS:based upon clinical manifestations. Cultures of blood, needle aspirations, or punch biopsies are usually not useful in the setting of mild infection.Blood cultures are positive in less than 5 percent of cases.
Cultures of blood, pus, or bullae are more useful and should be performed in patients with systemic toxicity, extensive skin involvement, underlying comorbidities (lymphedema, malignancy, neutropenia, immunodeficiency, splenectomy, diabetes), special exposures (animal bite, water-associated injury) or recurrent or persistent cellulitis.
MICROBIOLOGY — The vast majority of cases of erysipelas are caused by beta-hemolytic streptococci.
The most common cellulitis pathogens are beta-hemolytic streptococci (groups A, B, C, G, and F) and S. aureus, including methicillin-resistant strains (MRSA); gram-negative aerobic bacilli are identified in a minority of cases
TREATMENT:
Most patients develop mild cellulitis and can be treated with oral antibiotics; patients with signs of systemic toxicity or erythema that has progressed rapidly should be treated initially with parenteral antibiotics. Attention to dosing is important, particularly in obese individuals.
Treatment of cellulitis for neonates usually requires hospitalization and initial parenteral therapy, except for the mildest of cases. Empiric therapy must include coverage for group B streptococcus in addition to methicillin-resistant Staphylococcus aureus and other beta-hemolytic streptococci. Empiric parenteral therapy options include vancomycin plus either cefotaxime or gentamicin. Antibiotics that should be avoided in this age group include tetracyclines, trimethoprim-sulfamethoxazole, and ceftriaxone (cefotaxime is preferred over ceftriaxone). Dosing is weight- and age-based (table 1). Therapy is usually administered for 7 to 10 days.
Patients with purulent cellulitis (eg, cellulitis associated with purulent drainage or exudate, in the absence of a drainable abscess) should be managed with empiric therapy for infection due to MRSA, pending culture results.
Options for empiric oral therapy for treatment of MRSA include (table 2):
■Clindamycin
■Trimethoprim-sulfamethoxazole
■Tetracycline (doxycycline or minocycline)
■Linezolid or tedizolid
Patients with nonpurulent cellulitis (eg, cellulitis with no purulent drainage or exudate and no associated abscess) should be managed with empiric therapy for infection due to beta-hemolytic streptococci and MSSA.
Empiric antimicrobial therapy for nonpurulent cellulitis (including beta-hemolytic streptococci and MSSA but not MRSA)
Adults Children age >28 days
Oral therapy
Dicloxacillin 500 mg orally every six hours 25 to 50 mg/kg per day orally in four doses
Cephalexin* 500 mg orally every six hours 25 to 50 mg/kg per day orally in three or four doses
Clindamycin• 300 to 450 mg orally every six to eight hours 20 to 30 mg/kg per day orally in four doses
Intravenous therapy
Cefazolin* 1 to 2 grams intravenously every eight hours 100 mg/kg per day intravenously in three or four doses
Oxacillin 2 grams intravenously every four hours 150 to 200 mg/kg per day intravenously in four or six doses
Nafcillin 2 grams intravenously every four hours 150 to 200 mg/kg per day intravenously in four or six doses
Clindamycin• 600 to 900 mg intravenously every eight hours 25 to 40 mg/kg per day intravenously in three or four doses
Follow-up — Patients with cellulitis typically report symptomatic improvement within 24 to 48 hours of beginning antimicrobial therapy, although visible improvement of clinical manifestations may take up to 72 hours. Continuing extension of erythema or worsening systemic symptoms after this period of time should prompt consideration of resistant pathogens or alternative diagnoses.
RECURRENT CELLULITIS — Management of recurrent infection can be a challenging problem. In a study of 209 cases of cellulitis, recurrences were observed in 17 percent of patients.
The efficacy of prophylactic antibiotics for management of recurrent cellulitis is unclear, especially in patients with obesity(BMI>33), multiple episodes or lymphedema in lower extremities.
For known or presumed beta-hemolytic streptococcal infection, options for prophylactic antibiotics include monthly or bimonthly intramuscular benzathine penicillin injections (1.2 million units for patients who weigh >27 kg; 600,000 units for patients who weigh ≤27 kg) or oral therapy with penicillin V (250 to 500 mg orally twice daily). Staphylococcal infection prophylaxis may be attempted with clindamycin (150 mg orally once daily for adults) [66]. Staphylococcal prophylaxis for recurrent cellulitis is rarely necessary in children. Suppressive therapy may be continued for several months with interval assessment for relapse. Alternatively, patients may self-initiate antibiotic therapy immediately when symptoms of infection begin and seek medical attention.
SUMMARY AND RECOMMENDATIONS
■Cellulitis and erysipelas manifest as areas of skin erythema, edema, and warmth in the absence of underlying suppurative foci. Erysipelas has more distinctive anatomic features than cellulitis; erysipelas lesions are raised above the level of surrounding skin so that a clear line of demarcation between involved and uninvolved tissue is usually present. (See 'Clinical manifestations' above.)
■Predisposing factors include disruption to the skin barrier as a result of trauma (such as penetrating wounds or injection drug use), inflammation (such as eczema or radiation therapy), preexisting skin infection (such as impetigo or tinea pedis), and edema (due to venous insufficiency). (See 'Clinical manifestations' above.)
■The diagnosis of cellulitis is based upon clinical manifestations. Cultures are necessary only in patients with systemic toxicity, extensive skin involvement, underlying comorbidities, special exposures (animal bite, water-associated injury), or recurrent or persistent cellulitis. (See 'Diagnosis' above.)
■The most common causes of cellulitis are beta-hemolytic streptococcus (groups A, B, C, G, and F), and other pathogens include Staphylococcus aureus; gram-negative aerobic bacilli are identified in a minority of cases. Beta-hemolytic streptococci are the predominant cause of erysipelas. (See 'Microbiology' above.)
■Management of cellulitis and erysipelas should include supportive measures, such as elevation of the affected area and treatment of underlying predisposing conditions. (See 'Nonantibiotic therapy' above.)
■Most patients develop mild cellulitis and can be treated with oral antibiotics. We recommend that patients with signs of systemic toxicity or erythema that has progressed rapidly should be treated initially with parenteral antibiotics (Grade 1B). Initial parenteral antibiotics are also indicated for most neonates with cellulitis (table 1). (See 'Cellulitis' above.)
■Patients with nonpurulent cellulitis should be managed with empiric therapy for infection due to beta-hemolytic streptococci and methicillin-susceptible S. aureus (MSSA) (table 4). Patients with nonpurulent cellulitis and additional risk factors for MRSA (table 5) should be managed with empiric therapy for infection due to beta-hemolytic streptococci and methicillin-resistant S. aureus (MRSA) (table 6). (See 'Nonpurulent' above.)
■Patients with purulent cellulitis (eg, cellulitis associated with purulent drainage or exudate, in the absence of a drainable abscess) should be managed with empiric therapy for infection due to MRSA, pending culture results (table 2) . (See 'Purulent' above.)
■Patients with classic manifestations of erysipelas and systemic manifestations, such as fever and chills, should be treated with parenteral therapy. Patients with mild infection or those who have improved following initial treatment with parenteral antibiotic therapy may be treated with oral therapy (table 7). (See 'Erysipelas' above.)
■The duration of therapy should be individualized depending on clinical response; 5 to 10 days is usually appropriate; longer duration of therapy may be warranted in patients with severe disease. (See 'Follow-up' above.)
■We suggest administration of suppressive antibiotic therapy for patients with recurrent cellulitis who have predisposing factors that cannot be alleviated (Grade 2B). (See 'Recurrent cellulitis' above.)
2013年9月18日星期三
9-18-2013
Ancef cefazolin 1g iv q8h
Keflex cefalexin 1g iv q8h
healthcare acquired pneumonia
current treatment: vancomycin(15 to 20 mg/kg [based on actual body weight] intravenously every 8 to 12 hours)+ceftazidime(2 g intravenously every 8 hours)
Empiric treatment
No known multidrug resistance risk factors
one of the following intravenous antibiotic regimens
Keflex cefalexin 1g iv q8h
healthcare acquired pneumonia
current treatment: vancomycin(15 to 20 mg/kg [based on actual body weight] intravenously every 8 to 12 hours)+ceftazidime(2 g intravenously every 8 hours)
- Hospital-acquired (or nosocomial) pneumonia (HAP) is pneumonia that occurs 48 hours or more after admission and did not appear to be incubating at the time of admission.
- Ventilator-associated pneumonia (VAP) is a type of HAP that develops more than 48 to 72 hours after endotracheal intubation.
- Healthcare-associated pneumonia (HCAP) is defined as pneumonia that occurs in a non-hospitalized patient with extensive healthcare contact, as defined by one or more of the following:
- Intravenous therapy, wound care, or intravenous chemotherapy within the prior 30 days
- Residence in a nursing home or other long-term care facility
- Hospitalization in an acute care hospital for two or more days within the prior 90 days
- Attendance at a hospital or hemodialysis clinic within the prior 30 days
Empiric treatment
No known multidrug resistance risk factors
one of the following intravenous antibiotic regimens
- Ceftriaxone (2 g intravenously daily).
- Ampicillin-sulbactam (3 g intravenously every six hours).
- Levofloxacin (750 mg intravenously daily) or moxifloxacin (400 mg intravenously daily). When the patient is able to take oral medications, either agent may be administered orally at the same dose as that used for IV administration.
- Ertapenem (1 g intravenously daily)
ONE of the following:
- Antipseudomonal cephalosporin such as cefepime (2 g intravenously every eight hours) or ceftazidime (2 g intravenously every 8 hours).
- Antipseudomonal carbapenem such as imipenem (500 mg intravenously every six hours) or meropenem (1 g intravenously every eight hours) or doripenem (500 mg intravenously every eight hours; administered over one hour for HAP or HCAP, administered over four hours for VAP) [53,54].
- Piperacillin-tazobactam (4.5 g intravenously every six hours).
- For patients who are allergic to penicillin, the type and severity of reaction should be assessed. The great majority of patients who are allergic to penicillin by skin testing can still receive cephalosporins (especially third-generation cephalosporins) or carbapenems. If there is a history of a mild reaction to penicillin (not an IgE-mediated reaction, Stevens Johnson syndrome or toxic epidermal necrolysis), it is reasonable to administer a cephalosporin or carbapenem using a simple graded challenge (eg, give 1/10 of dose, observe closely for 1 hour, then give remaining 9/10 of dose, observe closely for 1 hour). Skin testing is indicated in some situations. If a skin test is positive or if there is significant concern to warrant avoidance of a cephalosporin or carbapenem, aztreonam (2 g intravenously every six to eight hours) is recommended. Indications and strategies for skin testing are reviewed elsewhere. (See "Penicillin-allergic patients: Use of cephalosporins, carbapenems, and monobactams".)
- Patients with past allergic reactions to cephalosporins may also be treated with aztreonam, with the possible exception of those allergic to ceftazidime. Ceftazidime and aztreonam have similar side chain groups, and cross reactivity between the two drugs is variable. The prevalence of cross-sensitivity has been estimated at <5 percent of patients, based upon limited data. Patients with past reactions to ceftazidime that were life-threatening or suggestive of anaphylaxis (involving urticaria, bronchospasm, and/or hypotension) should not be given aztreonam unless evaluated by an allergy specialist. In contrast, a reasonable approach in those with mild past reactions to ceftazidime (eg, uncomplicated maculopapular rash) would involve informing the patient of the low risk of cross-reactivity and administering aztreonam with a graded challenge (1/100, 1/10, full dose, each separated by 1 hour of observation).
- Antipseudomonal fluoroquinolone, preferred regimen if Legionella is likely, such as ciprofloxacin (400 mg intravenously every eight hours) or levofloxacin (750 mg intravenously daily). These agents may be administered orally when the patient is able to take oral medications. The dose of levofloxacin is the same when given intravenously and orally, while the dose of ciprofloxacin is 750 mg orally twice daily.
- Aminoglycoside such as gentamicin or tobramycin (7 mg/kg intravenously once daily) or amikacin (20 mg/kg intravenously once daily); once daily dosing is only appropriate for patients with normal renal function. A single serum concentration should be obtained 6 to 14 hours after the first dose, and the dose should be adjusted as needed based upon the following nomogram (figure 1). The aminoglycoside can be stopped after five to seven days in responding patients. (See "Consolidated aminoglycoside dosing with gentamicin and tobramycin".)
- Addition of an alternative agent, such as intravenous colistin, may be appropriate if highly resistant Pseudomonas spp or Acinetobacter spp is suspected (see "Treatment of Pseudomonas aeruginosa infections", section on 'Alternative therapy in multidrug resistant infections' and "Acinetobacter infection: Treatment and prevention", section on 'Pneumonia' and "Colistin: An overview", section on 'Systemic administration') [56]. In some cases, inhaled colistin may be appropriate as adjunctive therapy in combination with systemic antimicrobials, as discussed below.
- Linezolid (600 mg intravenously every 12 hours; may be administered orally when the patient is able to take oral medications)
- Vancomycin (15 to 20 mg/kg [based on actual body weight] intravenously every 8 to 12 hours for patients with normal renal function, with a target serum trough concentration of 15 to 20 mg/L.) In seriously ill patients, a loading dose of 25 to 30 mg/kg can be used to facilitate rapid attainment of the target trough concentration.
RECOMMENDATIONS FOR USE OF ZOSTER VACCINE
General recommendations — The zoster vaccine (Zostavax; Merck Pharmaceuticals) has been approved for use in the United States, Europe, and Australia. The United States Advisory Committee on Immunization Practices (ACIP) voted to recommend herpes zoster vaccination for all people aged 60 years and older in 2006 [20].
In 2011, the Food and Drug Administration (FDA) approved the use of zoster vaccine among persons 50 to 59 years of age based on preliminary efficacy data from a randomized clinical trial [19]. In June 2011 the Advisory Committee on Immunization Practices declined to recommend zoster vaccine in this age group, citing concerns regarding shortfalls of zoster vaccine for general use [21]. (See 'Adults 50 to 59 years of age' above.)
Zoster vaccine is NOT indicated for the treatment of zoster or post-herpetic neuralgia.
Formulation and administration — The zoster vaccine is a live-attenuated vaccine, which is administered as a one-time subcutaneous injection. The vaccine contains 18,700 to 60,000 plaque-forming units of virus, considerably more than the approximately 1350 plaque-forming units found in the Oka/Merck VZV vaccine for prevention of varicella [22].
Pneumococcal polysaccharide vaccine (PPSV, Pneumovax) and zoster vaccine should be separated by at least 4 weeks because the administration of PPSV may reduce the immunogenicity of zoster vaccine [23,24]. In situations where separating the vaccines by 4 weeks would be a barrier to vaccination, the Centers for Disease Control suggests giving the vaccines together [25,26]. This recommendation is based on data from an observational study that did not find a difference in the rate of herpes zoster among those who received the vaccines concurrently, compared to those who had the vaccines separated by 4 weeks [27].
Serologic testing — It is not necessary to elucidate whether the patient has a history of varicella prior to vaccine administration. Serologic testing for past exposure to VZV prior to immunization is also not required since it was not utilized in the large clinical trials described above [20,28,29].
The reader is referred elsewhere for details on the sensitivity and specificity of serologic testing. (See "Diagnosis of varicella-zoster virus infection".)
Use in patients with prior zoster — The Centers for Disease Control and Prevention and the ACIP recommend a single dose of zoster vaccine for adults aged >60 years, regardless of whether the patient has reported a prior episode of herpes zoster [30,31].
However, it is unclear if zoster vaccine offers any clear benefit among those with a recent history of herpes zoster. One retrospective study of 1036 vaccinated and 5180 unvaccinated persons >60 years of age with a history of zoster within the past four years found that the incidence of recurrent disease was low; only 29 well-documented cases were discovered on chart review during the 4.5 years of follow-up [32]. The low number of events precluded any definitive analysis of vaccine efficacy in prevention of zoster recurrence, though there was a trend toward lower rates among vaccinated patients. The scarcity of cases among persons with recent zoster may be related to endogenous boosting of VZV-specific T cells during reactivation disease.
Contraindications — Zoster vaccine is NOT advised for use in pregnant women or in individuals with a history of an anaphylactic reaction to gelatin or neomycin [33].
Zoster vaccine is also NOT advised in patients with primary or acquired immunodeficiencies (including leukemia, lymphoma, or other malignancies affecting the bone marrow or lymphatic system), AIDS, and patients on immunosuppressive therapies, since it is a live attenuated vaccine [34]. The use of zoster vaccine in the patient who is going to initiate immunosuppressive therapy is discussed below. (See 'Vaccination before immunosuppression' below.)
2013年9月17日星期二
9-17-2013
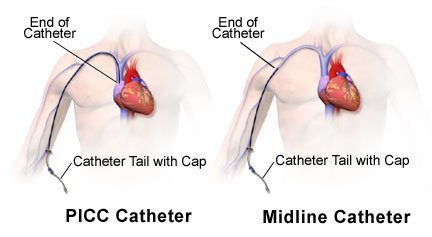
PICC lines enter a large central vein and a CXR is mandatory before the line is used to make sure that there is no pneumothorax and the line is in the correct place - in the distal portion of superior vena cava. PICC line can stay in place up to one year.
A midline is a 7-inch catheter (shorter than PICC) inserted in the antecubital region with the tip located in the axillary region. Thus CXR is usually not needed. Midlines can be used up to 4 weeks and that is why this catheter was chosen for the 2-week HIVAT course of this particular patient.
HIVAT (home IV antibiotics)
A midline is a 7-inch catheter (shorter than PICC) inserted in the antecubital region with the tip located in the axillary region. Thus CXR is usually not needed. Midlines can be used up to 4 weeks and that is why this catheter was chosen for the 2-week HIVAT course of this particular patient.
HIVAT (home IV antibiotics)
订阅:
博文 (Atom)