IJ vein landmarks

- Position patient in trendelenburg position (head angled down toward floor)
- Lower risk of air embolism
- Engorges vessels and allows for easier visualization
- Preparation of the catheter
- Flush all three central venous catheter lumens with Normal Saline
- Flushing lines is preferred to aspirating as low volume may result in line collapse on aspiration
- Preparation of skin
- Perform Ultrasound machine preparation and pre-scanning as above
- Position head extended and turned away from the insertion site
- Apply hibiclens to a wide area over the anterior-lateral neck
- Drape the neck to shield all but the prepped skin
- Local anesthetic
- Clear any air bubbles in a syringe of Lidocaine 1% without Epinephrine
- Air bubbles will markedly decrease quality of Ultrasound image
- Inject Lidocaine 1% without Epinephrine at the entry site
- Raise a skin wheal at insertion site
- Infiltrate along expected needle insertion tract
- Aspirate prior to injecting to prevent intravascular injection
- Clear any air bubbles in a syringe of Lidocaine 1% without Epinephrine
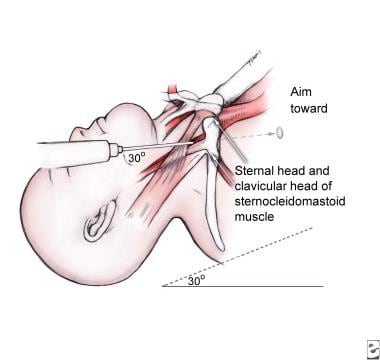
- Needle insertion site
- Use Ultrasound localization technique described above
- Insertion site
- Insertion site will be lateral to palpated carotid pulsation
- Approximately at top of triangle formed by sternocleidomastoid muscles bodies and clavicle
- Caution
- Internal Jugular Vein positioning is variable
- Ultrasound guidance is far preferred as landmarks are unreliable
- Avoid inserting needle through the sternocleidomastoid muscle (hematoma risk)
- Landmark triangle (insertion is at the apex of triangle, where two bodies of SCM meet)
- Anterior sternocleidomastoid muscle (SCM) body
- Posterior sternocleidomastoid muscle (SCM) body
- Clavicle (base of triangle)
- Landmarks by finger breadths
- Three fingers lateral to midline trachea
- Three fingers superior to clavicle (approximate level of cricoid ring)
- Needle insertion
- Needle types (either is attached to a 10 cc syringe)
- Steel Needle 18g (standard, more rigid)
- Angiocatheter 18g - long (alternative to steel needle)
- Angiocatheter (18 gauge) is typically included in the Central Line kit
- Once in lumen, remove needle and thread wire through catheter
- May be easier to maintain catheter within vessel lumen while threading guide wire
- In large patients, angiocatheter may be too short to access the vessel lumen
- Needle is directed toward nipple on side of insertion
- Insert needle at 45 degrees to the skin plane (when using Ultrasound guidance)
- Landmark insertion (without Ultrasound) is typically at a 30 degree angle to the skin plane
- Advance needle as described above under technique of Ultrasound-guided needle insertion
- Internal jugular is typically superficial (2-3 cm depth from skin surface)
- Aspirate while inserting needle
- Advance the needle another 0.5 cm past the time blood is first aspirated (to ensure in lumen)
- Needle types (either is attached to a 10 cc syringe)
- Guide-wire insertion
- Remove syringe from needle
- Occlude the open needle base to prevent bleeding and air embolism
- Insert guidewire
- Some recommend observing guidewire enter vessel on Ultrasound
- Typically insert guidewire until free end is approximately at the level of the patient's head
- Withdraw guidewire a short distance if ectopy seen on telemetry monitor
- Withdraw needle
- Firmly grasp guide wire
- Back out over the wire
- Adjust grasp on wire to be at skin entry site once needle is withdrawn
- Make skin nick
- Nick skin with #11 blade along the edge of the wire insertion site
- Confirm that the nick is contiguous with the space the wire lies within
- Dilator insertion
- Insert dilator over the wire and into the skin
- Do not fully insert dilator
- Only insert dilator far enough to dilate skin and soft tissue, but not vessel
- Twist the dilator to assist in advancing past resistance
- Withdraw the dilator
- Insert dilator over the wire and into the skin
- Central catheter insertion
- Always have hold of guidewire throughout this process
- Insert catheter over the guide wire via the longest, most distal port (remove brown cap)
- As catheter approaches skin, if guidewire does not emerge through port
- Withdraw the guidewire from skin until it emerges via port
- Grasp the guidewire at the distal port prior to letting go of guidewire at skin
- As catheter approaches skin, if guidewire does not emerge through port
- Advance catheter through skin to estimated depth
- Err on the side of caution by inserting further than estimate (e.g. 15 cm right, 20 cm left)
- Line may be withdrawn if inserted too far
- Line may not be inserted deeper after initial placement
- Deeper insertion requires replacement of line over another guidewire
- Typical final insertion depths (as above, insert further than these depths initially)
- Right side: Men 12-13 cm, Women: 11-12 cm
- Left side: Add 5 cm to right side length
- Err on the side of caution by inserting further than estimate (e.g. 15 cm right, 20 cm left)
- Remove guidewire
- Flush all 3 lines (all three lines should have been filled with saline in preparation)
- Confirm catheter placement
- Secure Central Line
- Portable Chest XRay
- Central Line tip should be at superior vena cava junction with right atrium
- Approximate tip position is 2 cm below the superior right heart sillhouette
- Tip will be 4-5 cm below the carina, just below the hilum
- Adjust Central Line based on Chest XRay (may withdraw, but may not insert further due to infection risk)
- Suture the Central Line in place





